A study was summarized by Robert Herpen, MA and Shenaz Bagha on the
American Epilepsy WebSite. The researchers, Xintian Lyn, BS, a student in the
department of experimental and clinical pharmacology at the College of Pharmacy
at the University of Minnesota and her team reported on their recent poster at
the American Epilepsy Society meetings earlier in December 2023 that adults
with epilepsy given medical cannabis had a significant decrease in weekly
seizure frequency.1
There is a paucity of data on the effects of THC (Tetrahydrocannabinol,
the principal psychoactive constituent of cannabis) on seizure frequency. This
researcher group in Minnesota was interested in cannabis’ effects on seizure
frequency.
From 2016 to 2019 one-hundred-twelve adults with epilepsy, 70% of whom
were aged 18-64 (54.5 % were male) were studied. The participants had at least
four visits for treatment for at least 6 months. They may or may not have had
antiseizure medications prescribed, too. The outcome of the study was that 57
participants reported fewer weekly seizures, 47 enrollees reported no
change—including 34 with zero frequency seizures during the study period—while
10 patients reported an increase in their seizure frequency. In all three of
these groups, participants were dispensed both CBD (cannabis) and THC. The
study found a significant difference reported in CBD total daily dose among
those who recorded either a decrease or no change in seizure frequency. CBD is
a chemical found in marijuana. CBD doesn't contain tetrahydrocannabinol (THC),
the psychoactive ingredient found in marijuana that produces a high.
Thirty patients relied on only CBD cannabis to manage their epileptic
seizures. Most of this study population were also taking one to five
antiseizure medications.
If your epilepsy is poorly controlled discuss adding CBD (cannabis) to
your treatment with your physicians. Additionally, explore the potential of
brain surgery as your epilepsy treatment if no other treatments benefit you.
Several of my previous 160 monthly blogs on my website: LanceFogan.com dealt
with brain surgery as a chance to improve your epilepsy when medications fail
(See Blog # 89 December 26, 2017: Surgical
Removal of Seizure Foci in Your Brain to Cure Poorly Controlled Epilepsy is
Safe!; Blog # 103 February 26, 2019: Epilepsy—fit
to drive?; Blog # 114 January 26, 2020: Epilepsy
surgery in childhood and long-term employment is encouraging.; Blog # 121
August 25, 2020: If
your seizures aren’t controlled epilepsy surgery is safe and really can help).
1. Lyu X. et al. Medical cannabis and seizure
control in Minnesota medical cannabis program. Presented at AmericanEpilepsy
Society annual meeting Dec. 1-5, 2023: Orlando, FL.
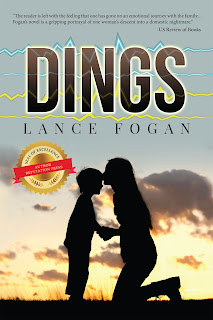
Lance Fogan, M.D. is Clinical Professor of Neurology at the David Geffen
School of Medicine at UCLA. His hard-hitting emotional family medical drama,
“DINGS, is told from a mother’s point of view. “DINGS” is his first novel.
Aside from acclamation on internet bookstore sites, U.S. Report of Books, and
the Hollywood Book Review, DINGS has been advertised in recent New York Times
Book Reviews, the Los Angeles Times Calendar section and Publishers Weekly.
DINGS teaches epilepsy and is now available in eBook, audiobook, soft and hard
cover editions.